Abstract
Low hemoglobin (Hb) level at steady state in subjects with sickle cell anemia (SCA) may indicate severe chronic hemolysis and might be related to a more severe course of disease.
In this study we investigated the hypothesis that low hemoglobin at steady state may be associated with higher rate of lung function impairment in children and adolescents with SCA.
Methods
In this cross-sectional study black African subjects with SCA (Hb phenotype SS) aged 6 to 18 years followed at the Barau Dikko Teaching Hospital, Kaduna, Nigeria, underwent spirometry and anthropometry measures. A recent Hemoglobin level at steady state was recorded for each patient. Caregivers or patients were interviewed through a questionnaire investigating a history of asthma or acute chest syndrome (ACS) and frequency of pain crises in the last year that required analgesics for at least 24 hours. Exclusion criteria were: the lack of recorded complete blood count (CBC) performed in the last 6 months, respiratory symptoms or feeling unwell on the test day, SCA-related acute events (e.g., pain crises) in the last two weeks or a blood transfusion or an ACS episode in the last month. A portable Easy-on-PC spirometer (ndd, Zurich, Switzerland) was used. Data were included if at least two forced expiratory manoeuvres met the ATS/ERS acceptability and repeatability criteria adapted for children (Miller MR, ERJ 2005; Kirkby J, Pediatr.Pulmonol.2008). Spirometry z-scores and percentage of predicted for FEV1, FVC and FEV1/FVC were derived according to the GLI-2012 reference equations for African Americans (Quanjer PH, ERJ2012). Spirometry patterns were classified as normal, obstructive (zFVC ≥ 1.64 + zFEV1/FVC < -1.64), restrictive (zFVC < -1.64 + zFEV1/FVC ≥ -1.64) or mixed (zFVC < -1.64 + zFEV1/FVC < -1.64) and a FEV1 < 70% of predicted was considered indicative of lung end-organ disease (Kassim AA et al, Blood. 2015 Sep 24;126(13):1544-50). Group comparison between patients with Hb level < 7.5 g/dL versus Hb ≥7.5 g/dL were tested using unpaired t test, χ2 or Fisher's exact test as appropriate. The relationship between Hb values and spirometry outcomes was explored through logistic and linear regression models. P-value < 0.05 was adopted as representing a statistically significant difference. Analyses were conducted using the software STATA and Graphpad Prism 7.
Results
A total of 186 subjects with SCA were initially enrolled. Only one child was on hydroxyurea. After exclusions, data from 126 patients (mean ± SD age of 11.5 ± 3.1 yr., 53% boys) were retained for the final analysis. Mean ± SD Hb value was 7.8±0.9 g/dL (range 5.6 to 10.9). Frequency of low Hb (< 7.5 g/dL) at steady state was 30.9% (39/126).
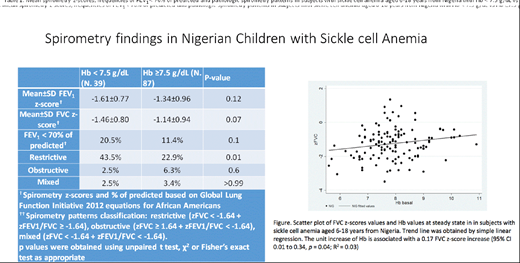
Mean FEV1 and FVC z-scores were lower and frequency of FEV1 < 70% of predicted was higher in patients in the low Hb group compared to those with Hb ≥7.5 g/dL though differences were not statistically significant (table 1). Prevalence of restrictive spirometry pattern, possibly suggesting restrictive lung disease, was significant higher in patients with Hb level < 7.5 g/dL (17/39, 43.5%) than in those with Hb ≥7.5 g/dL (20/87, 22.9%) (p = 0.01; table 1).
The odds ratio for restrictive spirometry pattern in presence of Hb level <7.5 g/dL was 2.5 (95% CI 1.1 to 5.7; p = 0.03). In a linear regression model (figure 1) the FVC z-score resulted significantly related to the Hb level with an increase of 0.17 z-scores for each point of Hb (95% CI 0.01 to 0.34, p = 0.04; R2 = 0.03).
Frequency of asthma, pain crises and previous acute chest syndrome did was similar between the two groups (data not showed)
Conclusions
In Nigerian pediatric patients with sickle cell anemia a hemoglobin level < 7.5 g/dL at steady state was associated with a 2.5 higher risk of presenting a restrictive spirometry pattern and with a higher frequency of end-organ lung disease (FEV1 < 70% of predicted). Low hemoglobin levels in wellbeing may depend on intense chronic haemolysis that could worsen microangiopathy, inflammation and ischemia and reperfusion injury in the lungs, potentially determining a precocious onset of restrictive lung disease.
These preliminary data seem to indicate that a low Hb level at steady state in African pediatric patients with sickle cell anemia is associated with more severe lung impairment and should prompt respiratory assessment with lung function when found.
Inusa:Novartis plc: Honoraria, Research Funding, Speakers Bureau; Astrazeneca: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal